It was a beautiful sunny day, not too hot with a nice cool breeze. As I jogged along the trail that passes through the meadow by my house, taking in the thousands of bright blue chicory flowers, I reflected on how lucky I am to live in such a beautiful place, to have a healthy body…. OUCH!
My knee was bugging me again, as it sometimes does when I’ve been running a lot without much cross training. Not that long ago I may have endured it, knowing that I would do some manual therapy or soft tissue work when I got home to try and coax my body back into a better alignment. Maybe I would have checked out my running form-making sure my core was engaged, and that my cadence was just right.
But today I know more. Thanks to the postural restoration institute, or PRI for short, I have such a deeper understanding of how so many things affect our movement and anatomy. I knew that the best thing I could do was just be more aware of the left side of the trail as it whizzed past. As I did that, my knee instantly felt much better.
Wait whaaaat??? Yup. Seriously. I simply became more aware of my left peripheral vision, which made my knee feel better.
Little disclaimer here…this is not to say that everyone who goes running will instantly be painfree by looking to the left, everyone has unique needs and nuances.
That said… it is a good idea to be aware of your peripheral vision when running and in general…more on that later.
But WHY??? Why would what I’m doing with my eyes affect my knee pain?
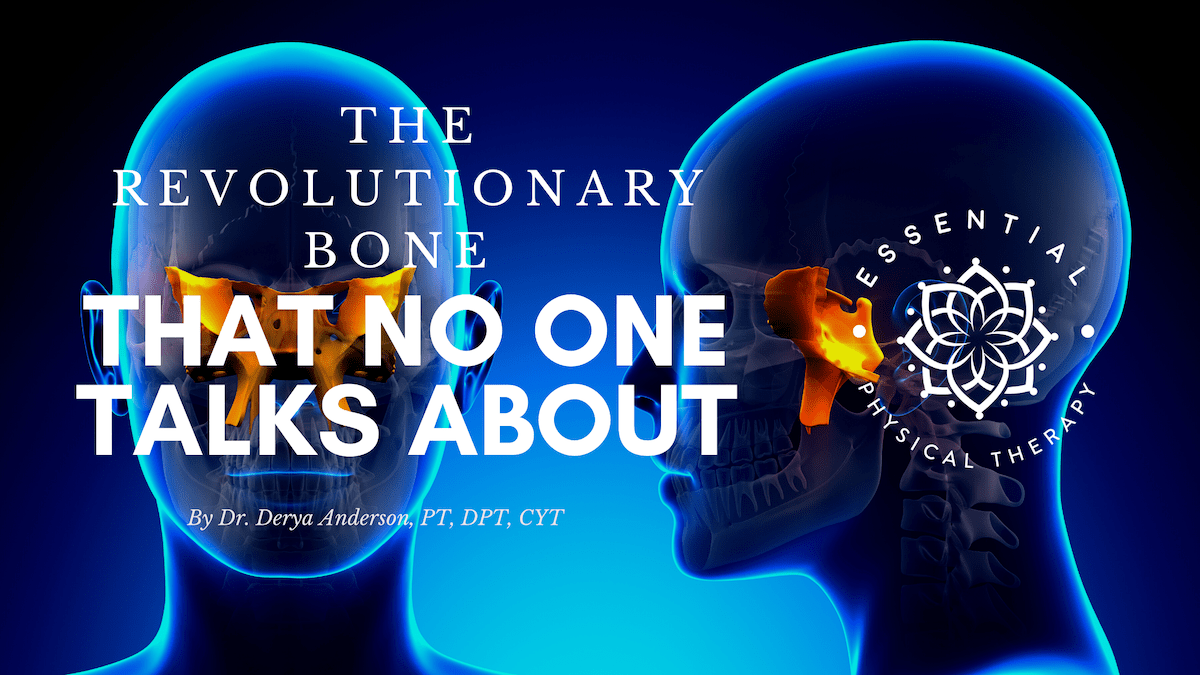
It’s all because of this special bone at the center of our head called the sphenoid.
Before we get into what this could possibly have to do with my knee, we should first ask ourselves…
Why Is the Sphenoid Bone So Special?
Here are just a few reasons…
- The sphenoid bone attaches to our jaw, our eyes, and our ears.
- The nerves that tell us to rest or digest or fight or flee or freeze pass through this bone.
- The main arteries that supply blood flow to your brain pass through this bone.
- The position of this bone determines the amount of pressure on your brainstem, which contains the apparatus to help your body organize movement.
- The pituitary gland, which performs life-sustaining functions, nestles nicely into a tiny protective saddle in the sphenoid bone.
I could keep going, but I think you get the point. This bone is responsible for a lot of important stuff!
Even just a tiny tweak in the position of the sphenoid could cause all sorts of repurcussions, many of which seem completely unrelated.
What Might Tweak a Sphenoid’s Position?
- The way your teeth touch matters big time to your sphenoid.
- The sphenoid interacts with your top and bottom teeth via muscles and nerve endings, but even the bony position of your jaw and maxilla (the bone that holds your top teeth) push against the sphenoid in certain ways. Not to mention, the periodontal ligament is HIGHLY sensitive to pressure and gives you lots of reference as to where you are in space. This neural information is then processed by your BRAINSTEM (remember that guy?) And what’s between your teeth and your brainstem? The sphenoid.
- Have you ever had dental work done and had the position of your tooth end up just a little higher or lower? If you have, you know it. Your body knows it. Everything feels off, you can’t relax until that tooth is back to where you like it! That’s the sensitivity of the periodontal ligament and the sphenoid position at play.
- Head injuries and concussions.
- I don’t think I really need to explain why a blow to the head can affect sphenoid position and surrounding function. But what most people don’t realize is that you don’t have to hit your head to get a concussion. Whiplash, blast exposure, falls, all these things can result in jostling the contents of the skull.
- How you use your eyes.
- Remember, the muscles that move your eyes around attach to your sphenoid. If you use your eyes the same way most of the time (like staring at a screen, for example), this can pull on the sphenoid.
- The neck.
- The poor head is at the whim of what the neck is doing. And the neck is at the whim of what the body is doing underneath it! Think of a house that is built on clay. When first built, everything is nice and level. But then, after a big rainstorm, different parts of the clay expand at different rates due to the moisture, and the foundation starts to shift and become unlevel. Of course everything above the foundation will also become unlevel. Similarly, if your body is imbalanced below your sphenoid, you will likely also have imbalance above.
Of course there are other situations where certain visual or dental changes (surgical or otherwise) can affect how you hold your body below, because, unlike a house, the body’s roof (the cranium) has just as much of an effect of where the foundation (rest of the body) sits due to all the sensory input we get from our head telling us where we are in space.
Don’t believe me? try standing on one foot. Got it? Good. Now try doing that with your eyes closed. Little harder? That’s because you’re getting information about where you are relative to the ground from your eyes, not just your feet.
Also, I have to say that if you had a head injury or dental work or vision work, this does not doom you to a life of a crooked sphenoid! It can certainly have an effect, but in most people it is manageable with the right program of manual therapy and movement techniques.
So back to my knee. Why did being aware of my left visual field help my knee?
At a purely structural level, there is some effect of letting my eye position change to pull on my sphenoid in a different way.
On a deeper, subtler, neurological level, being aware of the left does several powerful things.
Firstly, it reminds my body to become centered instead of pulling to the right, which I do (and most people do) because of our anatomy and the way our brains are wired. This is especially important for me since I have had a head injury which included broken facial bones.
Secondly, it opens up my left peripheral vision, which creates a sense of expansiveness in my body, thus allowing the sphenoid and surrounding bones to spread and widen. This takes pressure off of all those neural and vascular structures, and lets my body relax out of a state of tension.
When our bodies are held in a tense and protective state, we can’t rotate well through our torso. A side to side alternating activity like running absolutely requires the ability to rotate. If you can’t rotate at your trunk, your body will do it somewhere else. For me, it was my knee.
As soon as I let my left visual field soften and open, my body got a signal (or many signals, rather) to reposition itself into a more optimal position, subconsciously. I could rotate better, breathe better, and didn’t need to put any extra torque on my knee.
Well, I know this is a pretty heady conversation (get it? Heady? Skull? Ok I know, too punny) but it is one worth having.
Because sometimes you do all the right things and still aren’t feeling better or where you want to be with your sport, your breathing, your health, or your ability to do the things you want to do.
When that’s happening, it’s time to look at what’s happening from the neck up to determine if something there could be inhibiting your progress.
Here’s a simple but powerful technique to try that will help with restoring sphenoid position.